Neurofeedback in Psychological Practice
Author: Masterpasqua, Frank; Healey, Kathryn N. Source: Professional Psychology: Research and Practice December 2003 Vol. 34, No. 6, 652-656 ISSN: 0735-7028 Number: pro346652
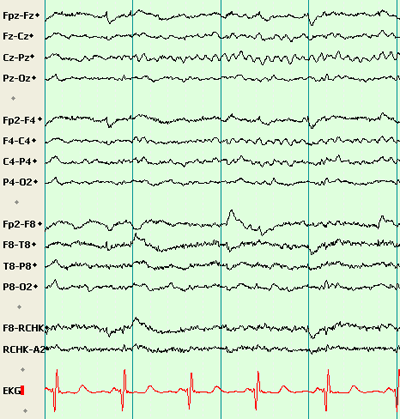
Neurofeedback, also known as EEG biofeedback or EEG operant conditioning, is an emerging modality with the potential of becoming an important part of effective psychological practice. Neurofeedback is a process whereby individuals learn to self-regulate their brain waves. Preliminary findings indicate that teaching individuals to alter electrocortical activity may have beneficial effects for attention-deficit/hyperactivity disorder (ADHD). Other research is ongoing to determine the effectiveness of neurofeedback for other disorders as well, including depression and schizophrenia. Its promise notwithstanding, neurofeedback has been virtually ignored by the mainstream investigators and clinicians. Even accounting for the absence of conclusive empirical efficacy, a process that combines two pillars of psychology-operant conditioning and brain function-deserves greater attention from the psychological community. With this article we hope to call attention to this modality by presenting some of the history and research pertaining to brain wave self-regulation.
A Brief History of Electroencephalography and Neurofeedback
Observations of electrical activity of the brain were first reported in 1875 when British physician Richard Caton observed electrical signals while probing the exposed cortices of animals. Fifty years later Hans Berger (1929) showed that electrocortical activity could be detected from the surface of the human scalp. It was Berger who first used the term electroencephalogram (EEG) and who identified different frequencies of brain waves measurable from the scalp. He also found that certain frequencies were characteristic of different states of attention. If subjects sat quietly with eyes closed, Berger observed frequencies around 10 cycles per second (10 Hz); if they were asked to focus on a mathematics problem with eyes open, frequencies were more likely to be in the range of 15 Hz.
Berger’s work encouraged others to determine whether particular features of an EEG were diagnostic for neurological or psychological disorders (see Robbins, 2000). Although there was some success linking EEG patterns to brain trauma and seizure disorders, early research was largely unsuccessful in relating EEG to psychopathology. Later in this article we report on more recent developments in the use of sophisticated techniques such as quantitative EEG (QEEG) that have revealed electrocortical correlates of a number of psychological and neurological disorders (Cantor, 1999; Hughes & John, 1999).
Following Miller’s (1969) seminal work demonstrating that autonomic functions can be operantly conditioned, psychologists were the first to discover that animals and humans could likewise learn to control their brain waves via contingent feedback (Robbins, 2000). A long series of studies by Sterman and his colleagues (Sterman & Friar, 1972; Sterman, Macdonald, & Stone, 1974) demonstrated that both cats and humans were able to learn to increase the amplitude of frequencies in the 12-15-Hz range recorded in the area of the sensorimotor cortex. Sterman (2000) found that patients with seizure disorders could use operant conditioning to increase these so-called SMR (sensorimotor rhythm) frequencies and thereby reduce seizure activity. As we report below, Sterman and Friar’s (1972)work with seizure disorders led directly to the first use of EEG biofeedback for ADHD (Lubar & Shouse, 1976).
At about the same time as Sterman and Friar’s (1972) work with frequencies in the 12-15-Hz range, Kamiya (1969) reported that the amplitude of slower brain waves in the 8-11-Hz range (so-called alpha waves) could also be increased through contingent feedback. Kamiya attached electrodes to the surface of the scalp to determine whether humans could correctly identify when there was a predominance of alpha waves (8-12 Hz) in the area of the occipital lobe. His participants were able to identify the state associated with alpha in relatively short order and were able to increase the amplitude of the alpha frequency when signaled to do so.
Kamiya’s (1969) work precipitated great interest in the operant conditioning of slower frequencies, both alpha and 4-7-Hz (theta), and the 1960s and 1970s witnessed a large number of studies designed to determine the efficacy of alpha/theta operant conditioning. Outcomes assessed ranged from enhancing peak performance, drug and alcohol abuse, and posttraumatic stress disorder (Evans & Abarbanel, 1999).
Neurofeedback could not withstand the multitude of claims made for its efficacy. The modality quickly became associated with the psychedelic, altered states of consciousness movement that was perceived as a fringe element of scientific psychology. It is not surprising then that it only required a few negative findings for neurofeedback to fall out of favor within the mainstream psychological community (Budzynski, 1999).
Neurofeedback in a New Technological Era
At about the same time that early efforts at EEG biofeedback were falling into disrepute, initial strides were being made in brain imaging techniques. In the past 20 years there has been a revolution in neuroscience, resulting in large part from advances in neuroimaging. Neuroimaging as well as progress in computerized neurophysiology, also known as QEEG, provide tools that may elucidate the mechanisms underlying neurofeedback.
Positron emission tomography (PET) and single photon emission computed tomography (SPECT) assess blood flow and activity patterns in the brain. The procedures require injection of small amounts of radioactive material that allow for visual representation of brain oxygen and glucose utilization. Functional magnetic resonance imaging is a more recent noninvasive technique that, along with PET scans, allows researchers to apprehend brain activity during cognitive tasks (see Sarter, Bernston, & Cacioppo, 1996).
In QEEG, electrodes are placed on multiple predetermined sites on the scalp, and data from these sites are submitted to computer analyses and “brain mapping.” The kinds of results available from conventional EEG and QEEG include but are not limited to distribution of electrical frequencies in various brain regions, the amplitude and shape of these frequencies, and the symmetry of frequencies, amplitudes, and wave shapes on homologous sites on each hemisphere. By comparing these measures to normative databases, researchers are able to identify brain wave patterns that are characteristic of various clinical populations.
On the basis of a review of over 200 studies, Hughes and John (1999) concluded that QEEG qualifies as an assessment tool for cerebrovascular disease, dementia, learning and attention disorders, mood disorders, postconcussion syndrome, schizophrenia, and substance abuse. In the discussion that follows, we show how some of these advances in EEG assessment are being used as the bases for neurofeedback interventions. We focus our discussion of the association between altered electrocortical activity and psychological disorder on ADHD and, to a lesser extent, depression. We do so because of recent work showing that each of these disorders can be distinguished by characteristic QEEGs and the existence of outcome studies implicating their responsiveness to neurofeedback.
QEEG and Neurofeedback for ADHD
QEEG evaluation.
Three independent research teams have now documented that individuals with ADHD can be differentiated from nonclinical samples by means of QEEG (Chabot & Serfontein, 1996; Janzen, Graap, Stephenson, Marshall, and Fitzsimmons, 1995; Monastra, Lubar, & Linden, 2001). Research consistently reveals that elevation in the average amplitude of slow brain wave frequencies (4-7 or 8-11 Hz) and a corresponding decrease in amplitude of higher frequencies (12-15 or 15-18 Hz), especially over the prefrontal or medial central cortex, is a distinguishing feature in ADHD subjects. These subjects show an even greater relative elevation in slow brain wave activity compared with faster activity when cognitively challenged (Lubar & Lubar, 1999).
The QEEG studies showing slower brain function among ADHD patients are corroborated by brain imaging research. Using PET scans, Zametkin et al (1990) reported a slowing of frontal cortex glucose metabolism in ADHD subjects. Much like the QEEG findings, those of Zametkin et al. showed that the slowing was especially noticeable during cognitive tasks. Using SPECT imaging, Amen and Carmichael (1997) also reported lower rates of metabolism in frontal and/or parietal lobes among their ADHD participants. Thus, the findings of relatively slower brain waves among subjects with ADHD are confirmed by brain imaging research showing relatively slower rates of metabolism at similar brain locations in similar populations.
The neurofeedback procedure.
Regardless of disorder, the neurofeedback procedure is relatively consistent across studies. Neuroelectrical activity is detected via surface electrodes; this activity is then amplified and processed by software programs that provide contingent auditory, tactile, and/or visual feedback to the patient via a game simulation on a computer monitor. For instance, a Pac-Man figure advances and sounds a tone whenever a client maintains waves in the 15-18-Hz range above a certain amplitude threshold while keeping waves in the 4-7 Hz range below a certain threshold. Amplitude thresholds are established for each individual so as to optimize motivation and learning. In this example, a reward would occur whenever the client maintains 15-18-Hz above predetermined amplitude 70% of the time while keeping the 4-7-Hz frequency above a predetermined amplitude only 20% of the time.
Outcomes using single-case designs.
Neurofeedback for ADHD began as an extension of Sterman and Friar’s (1972) groundbreaking work with epilepsy. Lubar and Shouse (1976) reasoned that increasing the sensorimotor rhythm through neurofeedback might serve to quiet motor responses in “hyperactive” children (as they were then called), much as it did for Sterman’s epileptic patients. Using a blinded ABA reversal design,Lubar and Shouse (1976) provided the first empirical evidence for the value of neurofeedback for ADHD. In this ABA design, a 9-year-old child first learned to improve EEG patterns and behaviors associated with ADHD (as assessed by observers who were blind to the procedure), then to return measures to baseline values, followed by a return to improved behavioral and EEG status. The authors reported that medication was permanently ended following the study and that the child continued to function well without medication long after the study’s termination. Using the blind ABA design with other children, Shouse and Lubar (1979) and Tansey (1993) replicated these findings. They also reported long-term positive effects of neurofeedback for these clients that lasted years after treatment, a finding with special significance, because the benefits of psychostimulants are known to last only while the patient is medicated.
Nash reviewed a number of other multiple-case studies (e.g., Alhambra et al., 1995; Tansey & Bruner, 1983; Thompson & Thompson, 1998 [all cited in Nash, 2000]) in which pre- and postneurofeedback assessments demonstrated improvements on measures including intelligence, academic skills, continuous performance tests, and behavioral rating scales.
Results of single-case designs and case studies can tell much about treatment effectiveness under real-world circumstances, but controlled studies comparing the treatment with placebo or other modalities are required to demonstrate efficacy of specific interventions (Chambless & Hollon, 1998). In the following section, we review results from published controlled group studies from four different research teams that are suggestive of a role for neurofeedback for ADHD.
Controlled group studies.
Rossiter and LaVaque (1995) compared neurofeedback and stimulant therapy in 46 patients (ages 8-21 years) who had self-selected participation in either neurofeedback or stimulant therapy conditions. Although assignments were not random, there were no significant pretest differences between groups on measures of age, gender, intelligence, ADHD subtype, frequency of other diagnoses, or type of school placements. The neurofeedback group received 20 sessions over a 3-month period; the medication-only group received doses of either methylphenidate or dextroamphetamine as prescribed by their personal physicians. Both neurofeedback and stimulant groups showed improvements from pre- to posttest on behavioral ratings completed by mothers using the Behavior Assessment Scale for Children (Reynolds & Kamphaus, 1992) and on a continuous performance measure, the Tests of Variables of Attention (TOVA; Greenburg & Dupuy, 1993). Results indicated positive effects for both medication and neurofeedback and an equal contribution from both therapies for symptom amelioration.
Linden, Habib, and Radojevic (1996) randomly assigned 18 patients (ages 8-21 years) to either a neurofeedback treatment or a wait-list control group. The treatment group learned to suppress theta (4-7 Hz) while enhancing beta waves during 40 sessions of feedback extending over 6 months. Neither group received medication. Compared with the control group, the neurofeedback group demonstrated significant pre- to posttest reductions in inattentive behaviors as assessed with the Swanson, Nolan, and Pelham (1988) measure and the Iowa Conners (Atkins & Milich, 1987) rating scales, as well as a significant increase in scores on the Kaufman Brief Intelligence Test (Kaufman & Kaufman, 1990).
Monastra, Monastra, and George (2002) compared the effects of Ritalin, EEG biofeedback, and parenting styles on the primary symptoms of ADHD in 100 children ages 6-19 years. All subjects participated in a 12-month comprehensive intervention that included Ritalin, parent counseling, and academic support at school. Fifty-one of the 100 children also received weekly sessions of neurofeedback modeled on the Lubar protocol designed to increase amplitudes in the 12-18 Hz range while decreasing amplitudes in the 4-11 Hz range at the central midline cortex (Lubar & Lubar, 1999). Pre- and posttreatment assessment included the Attention Deficit Disorders Evaluation Scales (ADDES, home and school versions; McCarney, 1995), TOVA, and a QEEG measure previously shown to distinguish children with ADHD (Monastra et al., 2001). No significant pretreatment differences existed for the two groups. After one year, children were assessed while taking Ritalin and while not taking the medication. While not taking Ritalin, only children who had received neurofeedback sustained the gains in the ADDES and TOVA. In addition, only children who received neurofeedback showed posttreatment improvement on the QEEG measure of neurophysiological changes. Thus, by “dismantling” the effects of neurofeedback from other forms of treatment, Monastra et al. (2002) demonstrated that only children who displayed changes in cortical arousal maintained improvements while not taking Ritalin and that only children who received neurofeedback training manifested those changes.
Fuchs, Birbaumer, Lutzenberger, Gruzelier, and Kaiser (2003) assigned 8-12-year-old children with ADHD to either a neurofeedback (n = 22) or methylphenidate (n = 12) condition on the basis of parents’ preference. The authors reported that both groups showed significant improvements on all subscales of the TOVA and on the d2 Attention Endurance Test (Brickenkamp, 1994). In addition, both groups showed significant declines in disordered behaviors as assessed by the German version of the Iowa Conners Behavior Rating Scale (Atkins & Milich, 1987). On all measures, improvements in outcomes from pre- to posttreatment were comparable between neurofeedback and methylphenidate.
In summary, four different research teams have performed controlled trials showing the efficacy of neurofeedback for ADHD. Each of these teams used a variation of Lubar’s original protocol designed to help children to increase frequencies ranging from 12-18 Hz while inhibiting frequencies in the 4-7 Hz or 8-11 Hz range. What is more, findings from one study (Monastra et al., 2002) suggested that neurofeedback provided for sustained changes in underlying EEG patterns, thereby indicating a potential mechanism for the effects of neurofeedback on behavior. Indeed, one of the implications of the Monastra et al study (2002) is that, unlike methylphenidate, neurofeedback’s benefits are retained when children are not receiving treatment. Although more research is required, we believe that these findings begin to demonstrate the role that neurofeedback can play in a multimodal approach to ADHD.
Neurofeedback for Other Disorders
It has been known for some time that damage to the left frontal lobe often leads to symptoms of depression, whereas damage to right frontal lobe is more likely to lead to symptoms of mania (Gainotti, 1972; Robinson & Downhill, 1995; Robinson, Starr, & Price, 1984). Recently, Davidson and colleagues (Davidson, 1993, 1994; Davidson, Jackson & Kalin, 2000) showed that alpha wave asymmetry between the frontal lobes can be diagnostic for mood disorders. Positive affect was associated with relatively lower amplitudes of frequencies in the 8-12 Hz (alpha) range in the left frontal cortex compared with the right frontal cortex. Conversely, negative affect corresponded to lower amplitudes of the alpha range in the right frontal compared with the left frontal lobes. Actively depressed patients as well as participants in current remission who had previously experienced depressive episodes showed relatively more left than right frontal alpha activity. The latter finding is consistent with a diathesis-stress model of depression, inasmuch as a person’s affective style appears to predispose him or her to depressive episodes.
Using alpha asymmetry as a starting point, Baehr, Rosenfeld, and colleagues sought to determine whether changing alpha asymmetry through neurofeedback could reduce symptoms of depression (Baehr, Rosenfeld, Baehr, & Earnest, 1999; Rosenfeld, 2000). In the Baehr et al. protocol, the subject hears a clarinet tone only when the amplitude of alpha (8-12 Hz) measured from the right frontal cortex is relatively greater than that of alpha measured from the left frontal cortex. Individuals were asked to maintain the tone and to increase its pitch for as long as possible during a session lasting 15-30 min. Baehr, Rosenfeld, and Baehr (2001) recently reported follow-up data on 3 of 6 depressed patients treated with the alpha asymmetry protocol. Patients showed positive changes in alpha asymmetry and on the Beck Depression Inventory both immediately after and 1-5 years following treatment. Similar clinical case studies (e.g., Hammond 2001; Rosenfeld, Baehr, Baehr, Gotlib, & Ranganath, 1996) are suggestive of the potential benefits of neurofeedback for the treatment of depression. Although a mechanism underlying the potential efficacy of neurofeedback has been articulated and clinical case studies are suggestive, controlled group outcomes are clearly required. Similar preliminary findings exist for other disorders, including schizophrenia (Gruzelier, 2000) and anxiety disorders (Moore, 2000).
Conclusion
It is not possible to make unqualified or categorical conclusions about the value of neurofeedback as a therapeutic modality. There are varying degrees of certainty about what is known. First, we have known for over 100 years that electrocortical activity can be measured and for over 50 years that different frequencies reflect different states of arousal. Second, we have known for 25 years that both animals and humans can learn to alter their brain waves through operant conditioning and thereby reduce seizures. Third, the work of Hughes and John (1999), among many others, documents that a number of psychological disorders, including ADHD, mood disorders, and schizophrenia, may be discriminated by characteristic patterns of the QEEG. Fourth, although still in its early stages, research documenting the efficacy of neurofeedback for ADHD is beginning to accumulate; four different research teams have demonstrated its efficacy using controlled trials. Finally, outcome research concerning the efficacy of neurofeedback for other disorders is still either experimental, or preliminary at best. On the basis of these findings, we suggest that clinicians begin to give greater consideration to neurofeedback as part of a multimodal approach, especially in the treatment of ADHD. We agree with Oubré (2002), who concluded the following:
Neurofeedback is perhaps best viewed not as an alternative to conventional psychopharmacological agents but rather as one component of a multimodal approach. When used as an adjunctive treatment in combination with standard medication, neurofeedback may improve clinical outcomes in some psychiatric patients. (p. 8)
It is also important to point out that the neurophysiological mechanisms purported to underlie neurofeedback are consistent with an emerging model in the neurosciences. This model is based on findings that timing of electrical activity throughout the brain and between various regions of the brain play a basic role in the emergence of psychopathology (Llinas, Ribary, Jenmonod, Kronberg, & Mitra, 1999; McCormack, 1999; Varela, Lachaux, Rodriquez, & Martinerie, 2001).
We encourage practicing psychologists to educate themselves more fully about the potential of neurofeedback; helping clients to learn to self-regulate neuronal function can become an important addition to psychological practice. Recent changes in billing codes include biofeedback (and EEG biofeedback) as reimbursable, either alone or in combination with psychotherapy. There are venues that provide clinicians with training, and most offer continuing education credits approved by the American Psychological Association. Private groups such as EEG Spectrum International (www.eegspectrum.com) and Thought Technology (www.thoughttechnology.com) offer introductory and advanced training in the skills necessary to begin to integrate neurofeedback into practice. In addition, the International Society for Neuronal Regulation sponsors the Journal of Neurotherapy and an annual conference. For those practitioners interested in referring their clients to clinicians trained in neurofeedback, the society’s Web site (www.snr-jnt.org) lists providers throughout the world. The Association for Applied Psychophysiology and Biofeedback focuses on the more general practice of biofeedback but includes a journal and annual conference that offer education in EEG biofeedback (www.aapb.org).
Unlike other biological treatment modalities, neurofeedback is steeped in the history and ethos of psychology. Especially for ADHD, practicing psychologists would do well to further educate themselves regarding the modality, as it shows promise as a therapeutic option in managing this condition.
References
Amen D. G., Carmichael B. D. High resolution brain SPECT imaging in ADHD., Annals of Clinical Psychiatry, Vol 9, 1997, 81-86
Atkins M., Milich R. Iowa Conners Teacher Rating Scale., In M. Hersen & A. Bellack (Eds.), Dictionary of behavioral assessment techniques(pp. 273-275). New York: Pergamon Press., 1987
Baehr F., Rosenfeld J. P., Baehr R., Earnest C. Clinical use of an alpha asymmetry protocol in treatment of mood disorders., In J. R. Evans & A. Abarbanel (Eds.), Introduction to quantitative EEG and neurofeedback(pp. 181-201). New York: Academic Press., 1999
Brickenkamp R. Test d2, Aufmerksamkeits-Belastungs-Test, (8th ed.). Gottingen, Germany: Hogrefe., 1994
Budzynski T. H. From EEG to neurofeedback., In J. R. Evans & A. Abarbanel (Eds.), Introduction to quantitative EEG and neurofeedback(pp. 65-79). New York: Academic Press., 1999
Cantor D. S. An overview of quantitative EEG and its applications to neurofeedback., In J. R. Evans & A. Abarbanel (Eds.), Introduction to quantitative EEG and neurofeedback(pp. 3-27). New York: Academic Press., 1999
Chabot R. J., Serfontein G. Quantitative electroencephalographic profiles of children with attention deficit disorder., Biological Psychiatry, Vol 40, 1996, 951-963
Chambless D. L., Hollon S. D. Defining empirically supported therapies., Journal of Consulting and Clinical Psychology, Vol 66, 1998, 7-18
Davidson R. J. Cerebral asymmetry and emotion: Conceptual and methodological conundrums., Cognition and Emotion, Vol 7, 1993, 115-138
Davidson R. J. Asymmetrical brain function, affective style and psychopathology: The role of experience and plasticity., Development and Psychopathology, Vol 6, 1994, 741-758
Davidson R. J., Jackson D. C., Kalin N. H. Emotion, plasticity, context, and regulation: Perspectives from affective neuroscience.,Psychological Bulletin, Vol 126, 2000, 890-909
Evans J. R., Abarbanel A. Introduction to quantitative EEG and neurofeedback., New York: Academic Press., 1999
Fuchs T., Birbaumer N., Lutzenberger W., Gruzelier J. H., Kaiser J. Neurofeedback treatment for attention-deficit/hyperactivity disorder in children: A comparison with methylphenidate., Applied Psychophysiology and Biofeedback, Vol 28, 2003, 1-12
Gainotti G. Emotional behavior and hemispheric side of lesion., Cortex, Vol 8, 1972, 41-55
Greenburg L. M., Dupuy T. R. Interpretation manual for the Tests of Variables of Attention computer program., Los Alamitos, CA: Universal Attention Disorders., 1993
Gruzelier J. Self regulation of electrocortical activity in schizophrenia: A review., Clinical Electroencephalography, Vol 31, 2000, 23-29
Hammond D. C. Neurofeedback treatment of depression with the Roshi., Journal of Neurotherapy, Vol 4, 2001, 45-56
Hughes J. R., John E. R. Conventional and quantitative electroencephalography in psychiatry., Journal of Neuropsychiatry and Clinical Neuroscience, Vol 11, 1999, 190-208
Janzen T., Graap K., Stephenson S., Marshall W., Fitzsimmons G. Differences in baseline EEG measures for ADD and normally achieving preadolescent males., Biofeedback & Self-Regulation, Vol 20, 1995, 65-82
Kamiya J. Operant control of EEG alpha rhythm and some of its reported effects on consciousness., In C. T. Tart (Ed.), Altered states of consciousness(pp. 519-529). New York: Wiley., 1969
Kaufman A. S., Kaufman N. L. Kaufman Brief Intelligence Test: Manual., Circle Pines, MN: American Guidance Service., 1990
Linden M., Habib T., Radojevic V. A controlled study of the effects of EEG biofeedback on cognition and behavior of children with attention deficit disorder and learning disabilities., Biofeedback & Self-Regulation, Vol 21, 1996, 35-49
Llinas R., Ribary U., Jeanmonod D., Kronberg E., Mitra P. P. Thalamocortical dysrhythmia: A neurological and neuropsychiatry syndrome characterized by magnetoencephalography., Proceedings of the National Academy of Sciences, USA, Vol 96, 1999, 15222-15227
Lubar J. F., Lubar J. O. Neurofeedback assessment and treatment for attention deficit/hyperactivity disorders., In J. R. Evans & A. Abarbanel (Eds.), Introduction to quantitative EEG and neurofeedback(pp. 103-143). New York: Academic Press., 1999
Lubar J. F., Shouse M. N. Use of biofeedback in the treatment of seizure disorders and hyperactivity., Advances in Clinical Child Psychology, Vol 1, 1976, 203-265
McCarney S. B. Attention Deficit Disorders Evaluation Scale., Columbia, MO: Hawthorne Press., 1995
McCormack D. A. Are thalamocortical rhythms the Rosetta stone of a subset of neurological disorders?, Nature Medicine, Vol 12, 1999, 1349-1351
Miller N. E. Learning of visceral and glandular responses., Science, Vol 163, 1969, January 31, 434-445
Monastra V. J., Lubar J. F., Linden M. The development of a quantitative electroencephalographic scanning process for attention deficit-hyperactivity disorder: Reliability and validity studies., Neuropsychology, Vol 15, 2001, 136-144
Monastra V. J., Monastra D. M., George S. The effects of stimulant therapy, EEG biofeedback, and parenting style on the primary symptoms of attention-deficit/hyperactivity disorder., Applied Psychophysiology and Biofeedback, Vol 27, 2002, 231-249
Moore N. C. A review of EEG biofeedback treatment of anxiety disorders., Clinical Electroencephalography, Vol 31, 2000, 1-6
Nash J. K. Treatment of attention deficit hyperactivity disorder with neurotherapy., Clinical Electroencephalography, Vol 31, 2000, 30-37
Oubré A. EEG neurofeedback for treating psychiatric disorders., Psychiatric Times, Retrieved July 1, 2002, from http://www.psychiatrictimes.com/p020268.html, Vol XIX, 2002
Reynolds C. R., Kamphaus R. W. Behavior assessment system for children., Circle Pines, MN: American Guidance Service., 1992
Robbins J. A symphony in the brain., New York: Atlantic Monthly Press., 2000
Robinson R. G., Downhill J. E. Lateralization of psychopathology in response to focal brain injury., In R. J. Davidson & K. Hugdahl (Eds.), Brain asymmetry(pp. 693-711). Cambridge, MA: MIT Press., 1995
Robinson R. G., Starr L. B., Price T. R. A two-year longitudinal study of mood disorders following stroke: Prevalence and duration at six months follow-up., British Journal of Psychiatry, Vol 144, 1984, 256-262
Rosenfeld J. P. An EEG biofeedback protocol for affective disorders., Clinical Electroencephalography, Vol 31, 2000, 7-13
Rosenfeld J. P., Baehr E., Baehr R., Gotlib I. H., Ranganath C. Preliminary evidence that daily changes in frontal alpha asymmetry correlate with changes in affect in therapy sessions., International Journal of Psychophysiology, Vol 23, 1996, 137-141
Rossiter T. R., LaVaque T. J. A comparison of EEG biofeedback and psychostimulants in treating attention deficit/hyperactivity disorder., Journal of Neurotherapy, Vol 1, 1995, 48-59
Sarter M., Bernston G. G., Cacioppo J. T. Brain imaging and cognitive neuroscience: Toward strong inference in attributing function to structure., American Psychologist, Vol 51, 1996, 13-21
Sterman M. B. Basic concepts and clinical findings in the treatment of seizure disorders with EEG operant conditioning., Clinical Electroencephalography, Vol 31, 2000, 45-55
Sterman M. B., Friar L. Suppression of seizures in epileptics following EEG feedback training., Electroencepalographic Clinical Neurophysiology, Vol 33, 1972, 89-95
Sterman M. B., Macdonald L. R., Stone R. K. Biofeedback training of the sensorimotor electroencephalogram rhythm in man: Effects on epilepsy., Epilepsia, Vol 15, 1974, 395-416
Swanson J., Nolan R., Pelham W. C. Swanson, Nolan, and Pelham Rating Scale (SNAP)., Pittsburgh, PA: Western Psychiatric Institute and Clinic, Department of Psychiatry., 1988
Tansey M. A. Ten-year stability of EEG biofeedback results for a hyperactive boy who failed fourth grade perceptually impaired class.,Biofeedback and Self-Regulation, Vol 18, 1993, 33-44
Varela F., Lachaux J., Rodriquez E., Martinerie J. The brainweb: Phase synchronization and large-scale integration., Nature Reviews: Neuroscience, Vol 2, 2001, 229-239
Zametkin A. J., Nordahl T. E., Gross M., King A. C., Semple W. E., Rumsey J. Cerebral glucose metabolism in adults with hyperactivity of childhood onset., New England Journal of Medicine, et al., Vol 323, 1990, 1361-1366
Caton R. The electric currents of the brain., British Medical Journal, Vol 2, 1875, 278
Berger H. Uber das electrenenkephalogramm des menschen, Archives von Pscyhiatrica Nervkrankh, [On the electroencephalogram of humans]., Vol 87, 1929, 527-570
Shouse M. N., Lubar J. F. Sensorimotor rhythm (SMR) and methylphenidate in the treatment of hyperkinesis., Biofeedback and Self-Regulation, Vol 4, 1979, 299-311
Baehr F., Rosenfeld J. P., Baehr R. Clinical use of an alpha asymmetry neurofeedback protocol in the treatment of mood disorders: Follow-up study one to five years post therapy., Journal of Neurotherapy, Vol 4, 2001, 11-18